This article was originally published on October 23, 2019, and has since been updated.
Corticosteroid injections are a way for people who have osteoarthritis—a degenerative joint disease in which the cartilage breaks down—to avoid oral steroids as a daily medication [1].
These injections are administered in joints such as the hip and knee so people who have painful arthritis can experience relief. Generally, the shots are done every few months and patients experience pain relief that could last anywhere from a few weeks to a few months.
Corticosteroid shots, within reason, have been considered a safe and popular treatment for people with arthritis. But a 2019 report, published in a journal called Radiology, reviews evidence and concludes that these injections can cause more damage to the joints than medical professionals previously thought [2].
Here’s what the research uncovered as well as how you might consider treating arthritis pain naturally.
Previously Known Risks of Corticosteroid Shots
Before getting a corticosteroid shot, as with most medical procedures, patients are required to review and sign a consent form acknowledging the risks of such a procedure.
What’s not on this form is the fact that these injections could actually cause hip and knee joints to degenerate faster, which could lead to premature hip and knee replacements. Generally, the procedure’s most common risks included on consent forms are infections (which are rare), allergic reactions, and bleeding at the site.
Getting injections into the same area over a period of time has also been shown to weaken tendons and bones, another risk patients should be aware of when opting for these shots [3].
What Complications the Research Discovered
The study reviewed the cases of 459 patients and found that 8 percent of them developed complications in the 15 months following their shots.
Of these 8 percent, 72 percent had moderate knee and hip osteoarthritis, and the patients had between 1 and 3 injections. Ages ranged from 37-79 [4].
Patients and doctors alike have previously thought that the injections weren’t harmful outside of their acknowledged risks, but the Radiology research reveals four additional, more significant concerns after reviewing the literature on the subject:
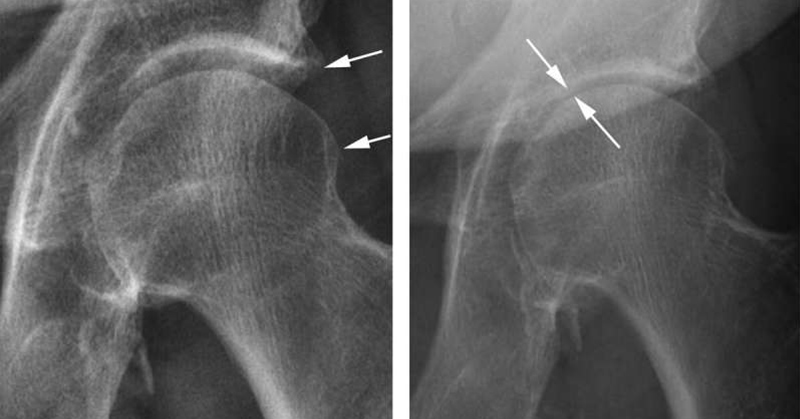
- Accelerated osteoarthritis with rapid loss of joint space. Narrowing of the joint space is typically indicative of cartilage loss but could point to other issues with the joint.
- Subchondral insufficiency fracture (SIF). A type of stress fracture that happens underneath the cartilage on the surface of a bone that bears weight. SIF was previously only thought to affect older patients receiving these injections, but the new research shows that younger patients are affected as well.
- Osteonecrosis. Also known as death of bone tissue, this has generally been an acknowledged risk of corticosteroid injections, which is interesting because these injections are often used to improve pain in those with osteonecrosis. However, given limited treatment options for osteonecrosis, sometimes these shots are the only option to relieve pain other than a joint replacement.
- Rapid joint destruction. Destruction of the joint due to progressive osteoarthritis can lead to joint collapse, which can cause sudden, severe pain in the joint.
The researchers concluded that these risks need to be presented to patients prior to determining whether or not corticosteroid injections are the most appropriate form of treatment for them.
The reason for these complications isn’t quite clear, but the authors suggest it’s possible that combining the drugs with a numbing agent could have a negative effect on the joints and cause cellular death.
Researchers Caution Physicians to Advise Patients
This isn’t the first time that the efficacy of these shots for joints has been questioned. Research dating back nearly a decade ago points to the fact that while corticosteroid shots can be an effective short-term solution, they might not be part of an appropriate long-term pain management strategy [6].
The authors of the study concluded that patients who have mild osteoarthritis—or osteoarthritis that doesn’t show up on imaging such as x-rays—don’t necessarily need these injections to resolve their pain, especially if their joint pain doesn’t add up with the image findings.
The authors also suggest additional diagnostics prior to getting the shots, as simple imaging techniques can sometimes reveal SIF and osteonecrosis prior to the injection, which could give patients more information about their risk.
In addition, the researchers note that the joint damage could have already been present prior to the shots, but wasn’t detected when the shots were done.
Patients with mild osteoarthritis in particular are at risk for developing one of the complications, including rapid degeneration of the joint or acceleration of osteoarthritis post injection. For these patients, other lifestyle changes such as diet and exercise may be a more appropriate approach to managing the disease.
People who have been newly diagnosed with osteoarthritis and are early along in the disease need to know the risks of these injections, the authors argue, instead of defaulting to corticosteroid shots as the best treatment simply because it’s common.
The Radiology study suggests that corticosteroid shots can aggravate arthritis or cause side effects that need to be better understood. They conclude that these injections are not without harm, and patients need to be made aware of the risks.
Are There Other Ways to Treat Osteoarthritis?
Yes! In fact, the best non-invasive way to manage osteoarthritis pain is with certain lifestyle changes. Hot and cold therapy, massage, supplements such as glucosamine, natural eggshell membrane (NEM), and exercise are all reputable ways to decrease arthritis pain and improve joint health [7].
Exercise is one of the best ways to treat arthritis pain and can help strengthen the muscles that work to support your joints. Good forms to try include swimming and biking—remember to start slow and gradually increase your regimen, working with your doctor or a physical therapist to customize an exercise program that works for your level of pain and mobility [7].
Foods that contain omega-3 fatty acids can also improve joint pain, especially wild-caught fish such as salmon and tuna, or plant-based sources such as flaxseeds and walnuts [7]. You may also consider taking a high EPA omega-3 supplement as well!
For many patients with arthritis, one treatment option won’t be enough to reduce pain and improve their quality of life, and some patients who experience extreme pain may need corticosteroid shots—the risks of which should be discussed in detail with your doctor, including any additional diagnostics, before your injection procedure!
Sources
- https://www.arthritis.org/about-arthritis/types/osteoarthritis/what-is-osteoarthritis.php
- https://pubs.rsna.org/doi/10.1148/radiol.2019190341
- https://my.clevelandclinic.org/health/treatments/4934-steroid-injections/risks–benefits
- https://www.nhs.uk/news/medication/steroid-injections/
- https://medicine.umich.edu/dept/orthopaedic-surgery/patient-care-services-hip-knee-replacement/osteonecrosis-or
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)61160-9/fulltext
- https://www.health.harvard.edu/pain/new-ways-to-beat-osteoarthritis-pain
- https://medicalxpress.com/news/2019-10-evidence-steroid-hip-knee-joints.html
Disclaimer: This information is not intended to be a substitute for professional medical advice, diagnosis or treatment and is for information only. Always seek the advice of your physician or another qualified health provider with any questions about your medical condition and/or current medication. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here.