Every year in the United States, 300,000 people die from sepsis.(2) This number is only on the rise, thanks to the aging population, drug-resistant bacteria, and weakened immune systems caused by HIV, cancer treatments, and transplant drugs. (1) We are now in a very serious situation that needs a solution, and quickly.
Anne’s Fritz’s father was her biggest fan. They shared everything together, all the good stuff and the bad. In November of 2009, he was the picture of good health as he walked her down the aisle. But by March 2010, he had died. That fall, a routine colonoscopy revealed that Anne’s father had polyps that were too large to remove during the procedure. There was a 40% chance that the polyps were cancerous, and that was too high of a risk for her father. The surgery was planned for February 2010, but was postponed until March of that year because of a giant snow storm that had hit Washington, D.C. area.
The surgery occurred on March 19 and it went well; the polyps were benign but her father had to stay in the hospital a while longer as he had a high heart rate and mild fever. After a week, her father was moved to a rehab center as he had lost a lot of strength from being bedridden at his age. Anne followed him to the rehab center where he met doctors, had his first rehab session, and then a nap. While being on oxygen, he was still in good spirits, alert, and talking to Anne. He soon fell asleep for a nap.
‘While he was sleeping, I went to the grocery store and back to his condo, where I made his favorite quiche to bring him for dinner. On my way back to see him, I stopped off at 7-Eleven for a Slurpee — a favorite treat of mine. When I got there, my dad asked for a taste, and wound up drinking the whole thing.’
Anne returned the next day with another quiche and a fresh Slurpee, but something was drastically different.
“When he asked me when we were going to the rehab center — the one we were currently sitting in — it was clear to me that something was very wrong. While he’d been weak the day before, he had his wits about him and had an appetite.”
She stayed with him all day that Sunday, and he was listless and tired, it was clear he wasn’t improving. She had to return to that night to New York where she lived but made sure to call as soon as she was back. She spoke to her father and he told her that the doctors were going to ‘take pictures of his tummy’, language that was not natural to him. She made sure her brother stayed on top of the medical team and followed up on the x rays.
After a terrible day at work on Monday worrying about her father, she returned home to the news that her father had died. The official cause of death was heart failure, but an autopsy revealed that his colon had been perforated during surgery, and the x rays would have shown the same thing, but they were never reviewed. The cause of her father’s death was sepsis.
Since then, Anne has learned that there was not much that she could have done to save her father. She learned that by the point he became confused, and even the day before, it likely would have been too late to reverse the course of the infection, experts say there is a 6-hour window in which something can be done. Unfortunately, this kind of thing happens more often than we might think.
Luckily, Dr. Paul Marik of the Sentara Norfolk General Hospital may have discovered a solution for just that. But first, an explanation of what sepsis actually is:
What is Sepsis?
Sepsis is a complication that comes from an infection, usually while the patient is still in the hospital. Sepsis occurs in three stages (1):
1. Sepsis
When you get an infection, your immune system releases chemicals into your bloodstream to fight back. Sepsis occurs when those chemicals trigger an inflammatory response throughout your entire body. To be diagnosed with sepsis, you must have at least two of the three following symptoms(1):
- Body temperature above 101F (38.3C) or below 96.8F (36C)
- Heart rate higher than 90 beats/minute
- Respiratory rate greater than 20 breaths/minute
2. Severe Sepsis
If left untreated, those chemicals cause changes in your body that damage your organs and eventually cause them to fail.
To qualify as severe sepsis, you must have one of the following signs of organ failure(1):
- Significantly decreased urine output
- Abrupt change in mental status
- Decrease in platelet count
- Difficulty breathing
- Abnormal heart pumping function
- Abdominal pain
3. Septic Shock
When severe sepsis progresses to septic shock, your blood pressure drops drastically. Organ failure plus extremely low blood pressure that doesn’t respond to fluid replacement means you have moved into septic shock.(1)
What are the Causes of Sepsis?
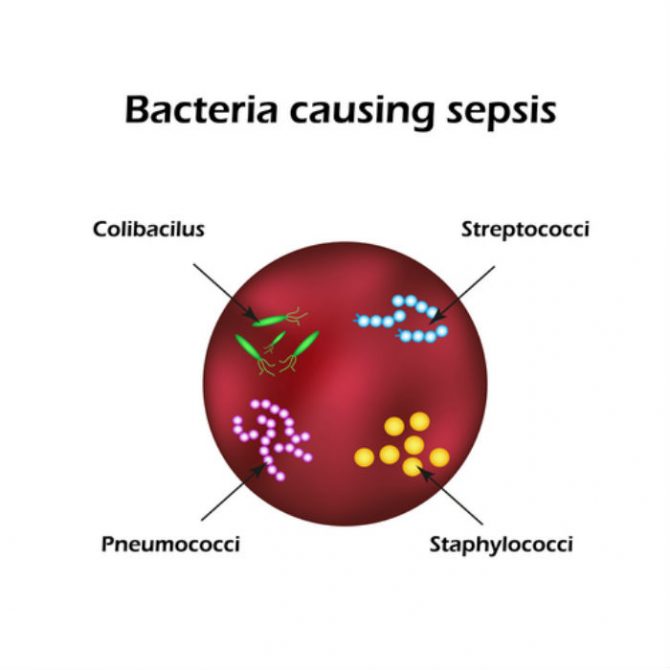
Any type of infection, whether it’s bacterial, fungal, or viral, can cause sepsis. The most common of these infections are:(1)
- Pneumonia
- Abdominal infection
- Kidney infection
- Bloodstream infection (bacteremia)
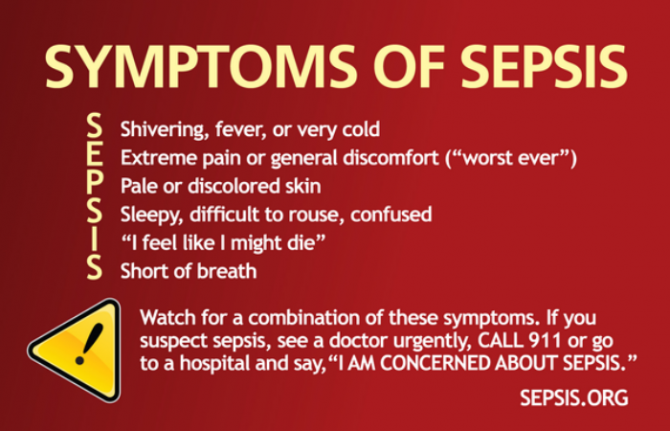
What are the Symptoms of Sepsis?
As you can tell from earlier, there are many different sepsis symptoms, and they are dependant on what stage you are in. Remember this acronym from sepsis.org to know what to look for:
Who is at greatest risk of sepsis?
Most healthy adults and children don’t have to worry about sepsis. Most often, sepsis and septic shock occur in older adults and those with weakened immune systems. You are at greater risk if you:(1)
- are very young or older (65+)
- have a compromised immune system (HIV, cancer treatment, transplant drugs)
- are already sick (patients in the ICU are highly vulnerable)
- have wounds or injuries such as burns
- are hooked up to invasive devices (intravenous, catheters, or breathing tubes)
Currently, there are no highly effective treatments for sepsis; mortality rate for septic shock is 50%.(2) This is why Dr. Marik’s discovery is an exciting development in the fight against this deadly disease.
The New Potential Sepsis Treatment
When a patient arrived in Dr. Paul Marik’s care who was nearing death from septic shock, he knew he had to think out of the box if he wanted to save her life. (3)
He had recently read a study by Virginia Commonwealth University that showed some success treating sepsis patients with intravenous vitamin c. Dr. Marik decided it was worth a shot. (3)
Along with the vitamin C, he added a low dose of corticosteroids and a small amount of the vitamin thiamine. To his amazement, this patient, who had multiple organs failing, survived. He tried this intravenous mixture with the next two patients he had with sepsis, and both lived. (3)
He has now treated 150 people this way, and only one of them died of sepsis.(3) That’s a far cry from the standard 50%!
Why this New Treatment is not Available Everywhere
With this exciting new development, it’s easy to want to jump ahead and use Dr. Marik’s solution in hospitals across the country. Even he agrees, however, the breaks need to be pumped a bit. Promising studies on sepsis treatment have been done before, only to then fail follow-up research.
It is important that every new treatment and drug for any disease go through the same rigorous testing before it is used.
This process looks like this:
- Animal testing
- Small group human trials
- Large group human trials
- FDA approval
In addition, the human trials must be done using a placebo, where both the participants and researchers don’t know which treatment they’re getting, and it must be done at several universities using several clinicians. This may take a long time, but it is critical in ensuring the safety and efficacy of every treatment that is developed before it is distributed on a mass scale.
Dr. Marik’s new treatment for sepsis is currently undergoing this process to fully understand the mechanism and be certain that it will work in different hospitals with different doctors.
Until the results of the new study are revealed, it is important that we are all vigilant in watching for the signs and symptoms of sepsis. If caught early, it can be treated with ease. If not caught until the patient is in septic shock, it will almost certainly be fatal. Join us in spreading the word to help protect the population from sepsis!

