This article was originally published on December 8, 2019, and has since been updated.
The heart is the primary life-giving organ in our bodies. When it stops beating, we die. But is it possible to bring it back to life? The world of medical science says yes.
In an exciting new trial, Doctors at Duke University Hospital in Durham, North Carolina, have successfully brought a “dead” heart back to life for the first time in the United States [1]. The transplant team at Duke was able to “reanimate” a heart and transplant it into a recipient through a process called Donation after Circulatory Death, or DCD [1].
How Are Heart Transplants Normally Done?

Heart transplant surgery is an open surgery and takes several hours. The process is fairly straightforward: a surgeon will make an incision in your chest, remove the diseased heart, and replace it with a donated healthy heart. He or she will then attach the major blood vessels to the heart. Usually, the heart will start beating as soon as blood flow is restored, but occasionally an electric shock needs to be applied to get the heart going again [2].
Donated hearts usually come from someone who is brain-dead but is still on life support [3]. The donor’s heart must be in good condition and be disease-free. It is also important that it matches as closely as possible with your blood type and tissue type so that your body does not reject your new heart [3].
The Long Wait for a Heart

About two thousand heart transplants are done in the United States every year [4]. Unfortunately, the waiting list to receive a transplant is very long, and patients usually have to wait more than six months before they get a surgery date [5].
This is important because the longer a patient has to wait for a new heart, the more likely that person is to die before they can get a transplant [6]. Research has also shown that the longer a person is on the waiting list for a new organ, the more likely it is for the transplant to fail [6].
Why is the list so long? Quite simply, there is a lack of donors. Dr. Jacob Schroder, who performed the transplant at Duke, explains:
“Currently, a conservative estimate would be that there are 250,000 people with end-stage heart failure who could theoretically qualify for a heart transplant,” he told CNN. “Due to the extreme lack of suitable donors, we only do 2,500-3,000 transplants per year using donation after brain death donors.” [7]
Less than half of Americans are registered as organ donors, and out of that number, only a small portion of those organs are actually usable [8].
Donation After Circulatory Death: A New Solution

In the past, a person had to be declared brain dead but still have a beating heart in order for their heart to be donated [1]. A DCD transplant does not have this requirement. This is how the procedure works:
- The heart stops beating and circulation ceases.
- There is a five-minute waiting period until the patient is declared dead.
- The heart is filled with a cold solution and is removed.
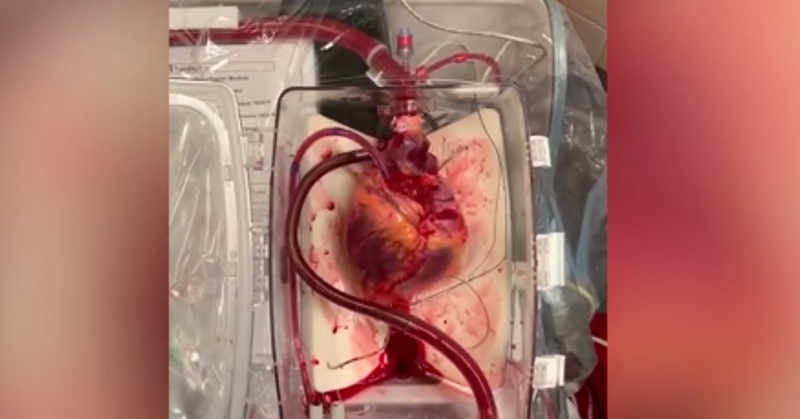
- The heart is placed into the TransMedics Organ Care System which gives the heart a supply of warm blood so it can beat again.
- Once the patient is ready, the heart is put back to “sleep” while it is being transplanted, and the transplant surgery continues as normal. [7]
DCD transfers have been used in the UK and Australia for a few years, but this is the first time in the United States [7]. This is very important for the future of heart transplants because it greatly increases the number of viable organs available, which could decrease the waiting list and ensure more people receive the transplants they so desperately need.
“This procedure has the potential to expand the donor pool by up to 30 percent,” said Schroder. “Increasing the number of donated hearts would decrease the wait time and the number of deaths that occur while people are waiting.” [1]
Read More: Sugar, Not Fat, is More Responsible for Heart Attacks, Doctors Says
Risks

There are some concerns with DCD transfers. “The major concern is that there is a period of time when the heart has no blood or oxygen getting to it prior to infusing it with the preservation solution and ice,” said Dr. Ashish Shah, the chair of cardiac surgery at Vanderbilt University Medical Center, who was not involved in the US transplant. “This period can vary considerably and may injure the heart permanently. That injury may not be seen until later, but it’s the one worry about using these organs.”
To determine whether or not the heart is still viable for transplant, doctors use what is called “warm ischemic time”. This is the amount of time that an organ or body part remains at body temperature after its blood supply has been reduced or cut off, but before it is cooled or reconnected to the body [9]. Compared to the other organs in your body, your heart has the lowest tolerance for warm ischemic time, and this time should not exceed thirty minutes [7].
A DCD Heart May be Better Than a Regular Heart
Dr. Pedro Catarino, director of transplantation at Royal Paperworth Hospital in the UK, says that in many cases, a DCD heart may be better than a standard heart because of the nature of donor-recipient matching [7].
“Consider the alternatives of a 50-year-old standard lady donor who died of a brain hemorrhage (often related to high blood pressure, which can also affect the heart). All her measures of heart function are good, and she is to all intents and purposes a ‘standard’ and good donor — picked up quickly by any center in the USA.” [7]
“In comparison, you may have a 20-year-old man who had a severe unrecoverable brain injury after an overdose but is not brain dead. Even after 30 minutes of injury, the younger, larger (male vs female) heart is likely to produce more ‘power’ than the former.” [7]
Next Steps

Of course, the procedure has its limitations. Patients must be in a hospital setting where doctors have control over timing, and there will need to be more expertise among recovery teams. [7] Despite some logistical roadblocks for DCD transplants, this new trial is still very exciting. There have been very few innovations over the last several years that could expand the donor pool, so this new procedure could have a profound impact on the future of heart transplants, and the lives that they save [7].
Read More: Doctors Brought Dead Heart ‘back to life’ For Groundbreaking Transplant
Sources
- “Doctors at Duke University Hospital Perform First DCD Heart Transplant.” Duke Health
- “Heart Transplant.” Mayo Clinic
- “Heart transplant.” Medline Plus
- “Cardiac transplantation in the United States: an analysis of the UNOS registry.” NCBI. Matthew J. Everly. 2008.
- “FAQ: Heart Transplant.” UCSF Health
- “Assessment of heart transplant waitlist time and pre- and post-transplant failure: A mixed methods approach.” NCBI. Benjamin A. Goldstein, PhD, et al. July 1, 2017
- “Doctors ‘reanimate’ heart for first-of-its-kind transplant in US.” CNN. Allen Kim. December 3, 2019.
- “Why Your Odds of Getting a Heart Transplant Are So Low.” Time. Emily Barone. November 30, 2017.
- “warm ischemia time.” National Cancer Institute