Dysphagia refers to a difficulty in swallowing – it takes more effort than normal to move food from the mouth to the stomach. Usually caused by nerve or muscle problems, dysphagia can be painful and is more common in older people and babies.
Although the medical term “dysphagia” is often regarded as a symptom or sign, it is sometimes used to describe a condition in its own right. There is a wide range of potential causes of dysphagia; if it only happens once or twice, there is probably no serious underlying problem, but, if it occurs regularly, it should be checked out by a doctor.
Read: Our Must-Buy Gifts For Grandma
Because there are many reasons why dysphagia can occur, treatment depends on the underlying cause.
In this article, we will discuss the various causes of dysphagia along with symptoms, diagnosis, and potential treatments, and a brilliant award-winning invention that can help older adults cope with the condition.
What is dysphagia?

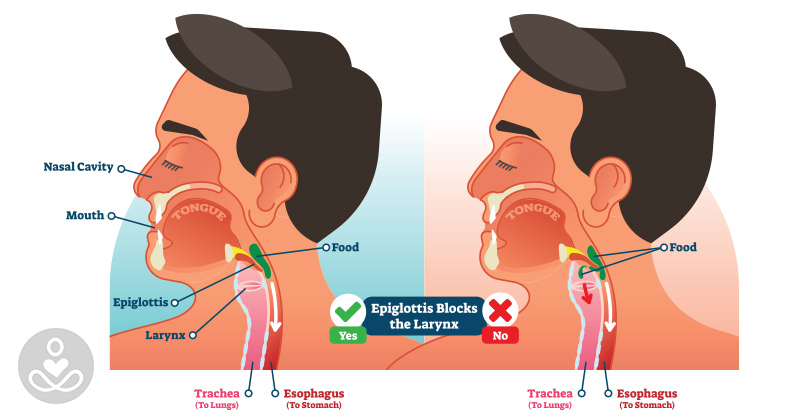
A typical “swallow” involves several different muscles and nerves; it is a surprisingly complex process. Dysphagia can be caused by a difficulty anywhere in the swallowing process.
There are three general types of dysphagia:
Oral dysphagia (high dysphagia) — The problem is in the mouth, sometimes caused by tongue weakness after a stroke, difficulty chewing food, or problems transporting food from the mouth.
Pharyngeal dysphagia — The problem is in the throat. Issues in the throat are often caused by a neurological problem that affects the nerves (such as Parkinson’s disease, stroke, or amyotrophic lateral sclerosis).
Esophageal dysphagia (low dysphagia) — The problem is in the esophagus. This is usually because of a blockage or irritation. Often, a surgical procedure is required.
It is worth noting that pain when swallowing (odynophagia) is different from dysphagia, but it is possible to have both at the same time. And, globus is the sensation of something being stuck in the throat.
Causes of dysphagia
Possible causes of dysphagia include:
Amyotrophic lateral sclerosis — An incurable form of progressive neurodegeneration; over time, the nerves in the spine and brain progressively lose function.
Achalasia —Lower esophageal muscle does not relax enough to allow food into the stomach.
Diffuse spasm — The muscles in the esophagus contract in an uncoordinated way.
Stroke — Brain cells die due to lack of oxygen because blood flow is reduced. If the brain cells that control swallowing are affected, it can cause dysphagia.
Esophageal ring — A small portion of the esophagus narrows, preventing solid foods from passing through sometimes.
Eosinophilic esophagitis — Severely elevated levels of eosinophils (a type of white blood cell) in the esophagus. These eosinophils grow in an uncontrolled way and attack the gastrointestinal system, leading to vomiting and difficulty with swallowing food.
Multiple sclerosis — The central nervous system is attacked by the immune system, destroying myelin, which normally protects the nerves.
Myasthenia gravis (Goldflam disease) — The muscles under voluntary control become easily tired and weak because there is a problem with how the nerves stimulate the contraction of muscles. This is an autoimmune disorder.
Parkinson’s disease and Parkinsonism syndromes — Parkinson’s disease is a gradually progressive, degenerative neurological disorder that impairs the patient’s motor skills.
Radiation — Some patients who received radiation therapy (radiotherapy) to the neck and head area may have swallowing difficulties.
Cleft lip and palate — Types of abnormal developments of the face due to incomplete fusing of bones in the head, resulting in gaps (clefts) in the palate and lip to nose area.
Scleroderma — A group of rare autoimmune diseases where the skin and connective tissues become tighter and harden.
Esophageal cancer — A type of cancer in the esophagus, usually related to either alcohol and smoking, or gastroesophageal reflux disease (GERD).
Esophageal stricture — A narrowing of the esophagus, it is often related to GERD.
Xerostomia (dry mouth) — There is not enough saliva to keep the mouth wet.
Editor’s Note: The following segment has been added to the original article to provide more information about a recent invention to help combat the effects of dysphagia.
Lewis Hornby saw firsthand the effects of dysphagia. His grandmother suffered from dementia, and he became well aware of how difficult it can be for seniors living with dementia and similar conditions to stay hydrated. So, he devised an ingenius tool: Jelly Drops.
Jelly Drops are bite-sized hydrating colorful pods which were designed to be more appealing to adults with dementia and easier to consume. Hornby explains:
“From my observations, people with dementia find eating much easier than drinking. Even still, it can be difficult to engage and encourage them to eat. I found the best way to overcome this is to offer them a treat!
This format excites people with dementia, they instantly recognize it and know how to interact with it. Jelly Drops builds on this insight – these bright, tasty treats attract the attention of people with dementia, and the firm, easy to grip ‘drops’ makes them simple to pick up.
The box itself contains many features to help people with dementia interact with it, and crucially it doesn’t look like a medical device. It’s friendly aesthetic reduces stigma around the solution, increasing its uptake.
When first offered, grandma ate 7 Jelly Drops in 10 minutes – the equivalent to a cup full of water, something that would usually take hours and require much more assistance. Eating the whole box would account for around half the necessary daily fluid intake.”
Jelly Drops won the Helen Hamlyn Design Award – Snowdon Award for Disability and Dyson School of Design Engineering DESIRE Award for Social Impact.