Ovarian cancer is the foremost cause of gynecological cancer death. It’s also extremely difficult to screen for and to diagnose at an early stage.
However, a controversial blood test exists that can measure the cancer antigen 125 (CA125) that can potentially detect ovarian cancer in its early stages. So why is it that ovarian cancer so difficult to screen for, and why is this test not more widely recommended?
The Statistics are Alarming
Approximately one in every 50 women will develop ovarian cancer. The rates are higher for women carrying the BRCA1 or BRCA2 gene mutations, up to 39%. (6) Only about 20% of ovarian cancers are found at an early stage, which is one of the main concerns for the high rates of death attributed to ovarian cancer. For any kind of cancer, the earlier the tumor is found, the greater chance the patient has for survival. (1)
There are two types of ovarian cancer. Type I carcinomas are slow-growing and are more common in Asia. Type II carcinomas are aggressive neoplasms and are more common in Europe and the United States. (4)
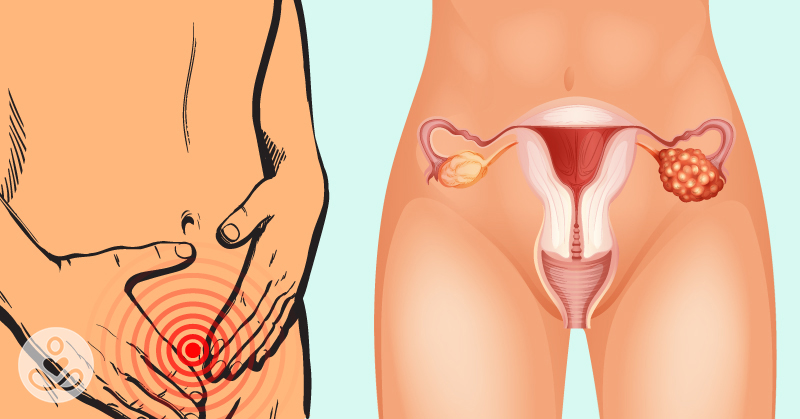
Ovarian Cancer Symptoms
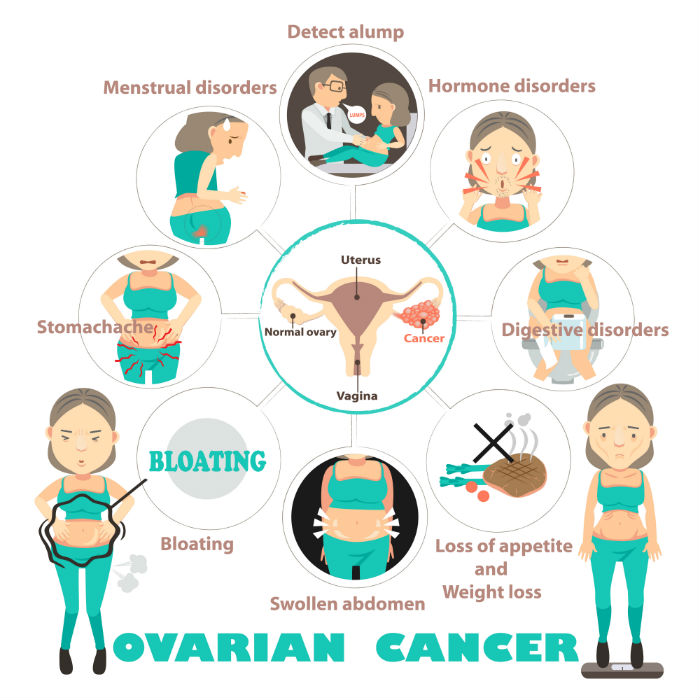
Ovarian cancer is called the “Silent Killer” because it is difficult to diagnose early, and because it often does not manifest any symptoms, especially in the early stages. Some of the symptoms include:
- Bloating
- Distended stomach
- Discomfort in stomach or pelvic area
- Loss of appetite
- Feeling full
- Frequent urination (1,2)
Those symptoms are often attributed to many different conditions, such as gastrointestinal issues. By the time ovarian cancer is diagnosed, often cancer has spread beyond the ovaries and into nearby organs.
Current Screening and Surgery Options
Gynecological screening is not beneficial to detect ovarian cancer. Traditional Pap tests are effective in early detection of cervical cancer, but not ovarian cancer. During a pelvic exam, the doctor can feel the ovaries and uterus for size, shape, and consistency, but it’s next to impossible for even the most skilled medical professional to find a tumor. (2)
High-risk women, including those with the BRCA mutation, are encouraged to have their ovaries and fallopian tubes removed as a precautionary surgery. The downside of this surgery is that it will push young women into early menopause, which will produce its own set of symptoms and issues.
Abby Lawson carries the BRCA1 mutation. At 33 years old, she opted to have the surgery, and I caught up with her prior to the operation. “Since I am done having my children, I am electing to have preventative surgery just in case, but that will also come with additional side effects. Part of me feels like a ticking time bomb, just waiting for cancer to rear its ugly head.”
Abby had the CA125 blood test performed every six months for the past several years, and watched the CA125 marker inch up past the recommended levels. “For me, the numbers weren’t high enough to prompt the doctors to do anything, but it was stressful watching the rise every few months and not know whether they were really an indication of cancer or if any of several other factors that could affect them was the culprit.”
What is the CA125 Test?
CA125 is a glycoprotein in the tissues throughout the body. In many women with ovarian cancer, levels of CA125 are high, particularly in ovarian cancer cells. A simple blood test of CA125 levels is used as an aid to help find tumors for an early diagnosis of ovarian cancer, and also as a marker to monitor potential ovarian cancer. (2,3,5)
While CA125 is used to help detect ovarian cancer, there are other cancer types that can cause higher than normal levels of CA125:
- Endometrial cancer
- Fallopian tube cancer
- Pancreatic cancer
- Stomach cancer
- Esophageal cancer
- Colon cancer
- Liver cancer
- Breast cancer
- Lung cancer. (3)
In addition to the cancers listed above, higher levels of CA125 can also be caused by the following conditions:
- Uterine fibroids
- Endometriosis
- Lupus
- Liver disease
- Pancreatitis
- Pelvic inflammatory disease
- The first trimester of a pregnancy
- Menstruation. (3)
Why is the CA125 Controversial?
During a clinical trial for CA125, Annwen Jones, the chief executive of Target Ovarian Cancer said, “An effective screening program for women at high risk of ovarian cancer due to family history would potentially have a major impact on mortality and survival from this disease.” (1)
The CA-125 blood test helps doctors:
- Monitor ovarian cancer and other cancers to determine if they are responding to treatment
- Monitor patients with ovarian and other cancers post-treatment to check for cancer recurrence
- To an extent, screen for ovarian cancer in women who are at high risk for developing the disease. (3)
According to Naturopathic Oncologist Dr. Heather Paulson, “The downside of using CA125 as a screening tool is that sometimes it is not elevated until advanced stages of ovarian cancer. In fact, 50% of women with Stage 1 ovarian cancer will have normal CA125 levels. Just because CA125 is normal doesn’t mean that there is no ovarian cancer present. On the flip side, elevated CA125 does not confirm ovarian cancer. It can be elevated due to fibroids, abdominal inflammation, endometriosis, and ovarian cysts.”
In studies of women at average risk of ovarian cancer, using CA125 for screening led to more testing and sometimes more surgeries, but did not lower the number of deaths caused by ovarian cancer. Because the CA125 test is still inconclusive, no major medical or professional organization recommends the routine use of CA125 blood test to screen for ovarian cancer. (2)
CA-125 in the US vs UK
The United States Food and Drug Administration recommended: “against using currently offered [CA125] tests to screen for ovarian cancer.” Additional concerns are that the blood test will prolong women having preventative surgery. (1)
For Abby, her CA125 was consistently above normal levels, but there was no significant jump. The test was inconclusive and caused extra stress. “Even though that’s the case, I am so, so thankful for technology that allows us to screen for things like BRCA genetic mutation and, armed with that knowledge, take strides to prevent cancer before it happens.”
The United Kingdom is more progressive with CA125 screening. In one clinical trial, CA125 levels were monitored and screening proved to detect ovarian cancer early. In another trial, the overall average mortality was reduced by 20%. Additional studies reported that the CA125 screening was associated with decreased staging at detection. (1,4)
It’s a Personal Decision
It’s still uncertain whether the CA125 test will detect ovarian cancer and if the screening will increase a woman’s chance of survival. “Finding ways to detect ovarian cancer earlier is a key to improved survival rates and treatment,” advises Dr. Paulson. “CA125 as a screening tool offers the benefit of being low cost and easy to administer. Overall, it seems too soon to recommend CA125 as a stand-alone screening test for ovarian cancer, but for a patient with a strong family history or genetic mutations I would encourage regular CA125 blood draws.”
At the end of the day, women still need to weigh the risks and benefits of surveillance or preventative surgery. The pathology from Abby’s surgery came back clear, and she is now breathing a sigh of relief. She wants “to have the best chance of being around to watch my children grow up and to experience a long, happy life.”
Sources
- https://www.bbc.co.uk/news/health-39103629
- https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/detection.html
- https://www.cancercenter.com/treatments/ca-125-test/?source=GGLPS01&channel=paid+search&invsrc=Non_Branded_Paid_Search_Google_General_Search&utm_device=c&utm_budget=Corporate&utm_site=GOOGLE&utm_campaign=Non+Brand%3ETreatments&utm_adgroup=Diagnostics%3ECA-125+Test%3EExact&utm_term=ca125+test&utm_matchtype=e&k_clickid=0848097b-41c6-4f97-9d7d-54edb161ea4e&k_profid=422&k_kwid=507045
- https://www.ncbi.nlm.nih.gov/pubmed/28257098
- https://www.ncbi.nlm.nih.gov/pubmed/28050675
- https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet#q2