For decades, the idea of regenerating damaged organs felt like science fiction. The idea was reserved for Star Trek episodes where a single pill could grow a new kidney. While scientists at Scripps Research faced many setbacks, that vision is finally inching toward a reality. Researchers have made breakthroughs in regenerative medicine: “tricking” the body’s innate repair systems. Using stem cells, they have managed to coax the cells into repairing organ damage. Unlike older methods that extract and reprogram stem cells in labs, this technique stimulates the body’s innate repair mechanisms.
Illnesses like pulmonary fibrosis, heart failure, and osteoarthritis cause damage to crucial organs like the heart and lungs. Usually, doctors would look at therapies to alleviate symptoms and stop the damage from worsening. Now, after 30 years of research and tests, they have potentially made a breakthrough that could give the body its own healing factor.
What Makes Stem Cells Special

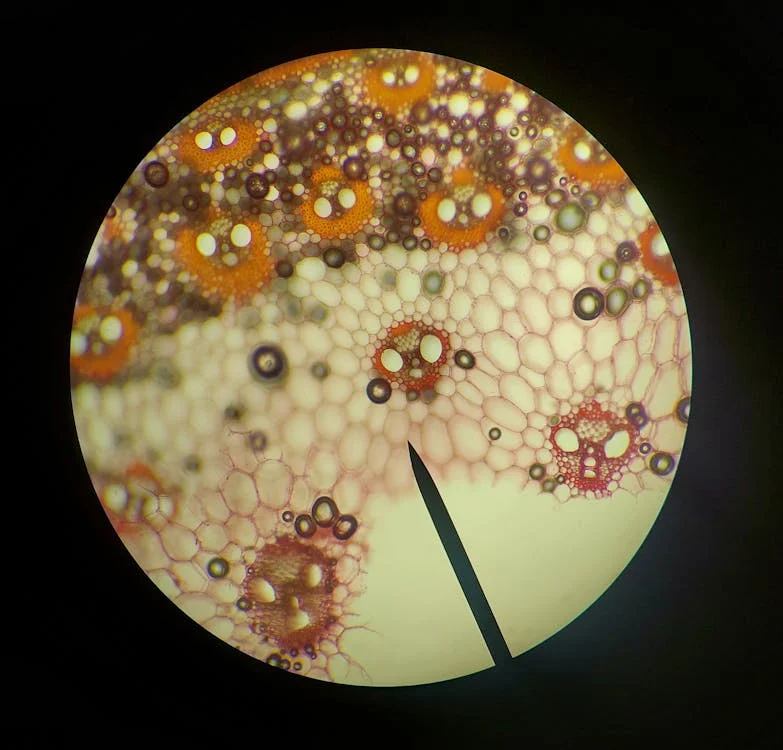
Scientists have long been captivated by stem cells for uses in regenerative medicine. Stem cells are coveted for their unique ability to differentiate into any cell type, acting as the body’s repair crew. Traditional approaches focused on extracting these cells, reprogramming them in labs, and re-implanting them. This process was plagued with technical and ethical issues, making research almost impossible. Now, a paradigm shift is underway.
Scientists at Scripps Research in California are bypassing lab manipulation entirely. Instead, they are developing drugs that activate endogenous stem cells, those already residing in organs, to regenerate tissue. “Our goal is to hand patients a pill or inhaler that kickstarts their body’s own repair mechanisms,” says Pete Schultz, CEO of Scripps. This approach recently restored function in scarred lungs and repaired heart muscle, showing promise for regenerative medicine.
Read More: In World First, Stem Cell Therapy Reverses Type 1 Diabetes in Patient
Breathing New Life into Damaged Tissue

Chronic lung diseases like idiopathic pulmonary fibrosis (IPF) and COPD affect over 500 million globally, often leaving patients reliant on oxygen tanks or lung transplants. Over 16 million Americans have COPD, and current treatments only ease symptoms. Scripps developed a breakthrough inhalable drug called CMR316 that targets type 2 alveolar epithelial (AEC2) cells.
The drug regenerates gas-exchange tissue, reversing scarring in mice and pigs. In mouse studies, weekly doses of the drug reduced fibrosis by 50% within a month, restoring healthy tissue. Human safety trials began in 2024, with plans to enroll IPF patients by late 2025. Yale researcher Maurizio Chioccioli, who maps lung stem cell behavior, calls the approach “transformative” but cautions that human biology may respond differently: “We’ve seen stem cells migrate and reshape during repair, factors we must account for.”
Healing Hearts After Attack

Heart disease remains the world’s leading cause of death, often leaving survivors with permanent scars that current medicine cannot repair. Scripps’ cardiac therapy uses a hydrogel injected into the pericardium (the heart’s protective sac) to reactivate dormant stem cells. In pigs, the treatment restored 30% of lost function post-heart attack, enough to transform a debilitated heart into one capable of normal activity.
Cardiologist Richard Stack, who advises Scripps, notes the stakes: “Current treatments save lives but don’t repair damage. Regrowing functional tissue would be a quantum leap.” Human trials are slated for 2027, pending FDA approval.
Challenges and Competing Approaches

Not all organs prove equally responsive. A Scripps drug designed to regenerate knee cartilage failed human trials in 2024, despite its success in animals. “Joints have a complex cellular environment. What works in mice doesn’t always translate,” explains Schultz. The injected drugs didn’t last long enough in joints to make meaningful differences. This setback highlights an important factor: organs stem cells’ responses vary from organism to organism, meaning treatment requires tailored responses.
Read More: Fat Cells ‘Remember’ Obesity, Offering Clues to Why Weight Loss is So Challenging
How Scripps Discovers These Treatments

At Scripps Research, scientists began an ambitious screening process entailing testing millions of potential drug molecules. The objective was to find compounds in the drug molecules that could activate the body’s dormant repair cells. The team specifically looked for molecules capable of stimulating endogenous stem cells, those naturally residing within organs, rather than relying on external transplants.
Their efforts paid off. Researchers successfully identified compounds that expand healthy stem cell populations in critical organs, particularly the lungs, heart, joints, and eyes. This discovery represents what Chuck Murry, director of USC’s regenerative medicine center, calls “a giant step toward the famous Star Trek scene” where Dr. McCoy hands a patient a single pill to grow a new kidney.
The approach builds on earlier collaboration between Scripps and the Novartis Research Foundation. They pioneered using small molecules to activate stem cells directly within the body.. This marks a departure from conventional regenerative medicine practices. Traditional methods required extracting stem cells, reprogramming them in laboratories, and surgically reimplanting them. This was a complex, expensive process with limited scalability.
“Drug-based activation is revolutionary because it’s accessible,” explains Schultz. “Instead of requiring specialized surgical centers, patients could receive treatment through simple pills or inhalers, reaching millions who need repair therapies.”
Read More: Scientists Have Successfully Grown ‘Mini Kidneys’ and Implanted Them Into a Live Subject
Reprogramming Cells for Transplants

While Scripps focuses on in-body repair, others are refining traditional stem cell methods. At the University of Southern California, Chuck Murry’s team reprograms blood stem cells into cardiomyocytes (heart muscle cells). In monkeys, transplanted cells integrated with no issue, beating in sync with the existing tissue. “Lab-grown cells let us patch specific damaged areas,” Murry says. However, this method requires surgery and carries rejection risks. Human trials are slated for 2027.
Ethical and Safety Hurdles

Stem cell therapies have a tainted reputation due to their past, marred by unproven “miracle cures” and fraudulent clinics. While current researchers emphasize rigorous testing, a major concern amongst scientists is cancer risk. Overstimulating stem cells could trigger uncontrolled growth or cancer. However, scientists remain confident by the lack of any adverse reactions to the treatment in smaller safety studies. Research in pigs found no abnormal cells in the heart or other organs.
The real challenge is figuring out where, when, and how much to activate pathways. Treatments must enhance repair without triggering adverse reactions. New heart cells must sync perfectly with existing tissue to prevent dangerous heart arrhythmias. Trials now prioritize safety, with longer-term human studies needed to confirm benefits.
Read More: Innovative Treatment Heals Spinal Cord Injuries by Triggering Special Proteins
Why This Matters
If successful, these therapies could transform treatment for diseases like COPD, pulmonary fibrosis, and heart failure. These are conditions where halting damage is currently the best option for treatment. As Pete Schultz, Scripps’ CEO, notes, “Reversing damage will fundamentally change how we think about treating disease”. However, safety concerns, such as avoiding cancerous overgrowth of activated cells, require more insight and caution.
Cautious Optimism

If trials succeed, the first regenerative drugs could debut by 2035, initially targeting terminal conditions like IPF. Costs remain a question, though Schultz predicts insurers will cover treatments that reduce long-term care needs. For millions with chronic diseases, the promise of repair, not just management, offers a lifeline. As Murry puts it: “We’re not just prolonging life. We’re rewriting what medicine can achieve.”
Read More: Goodbye Fillings? Teeth Have Been Successfully Grown in a Lab

