Want healthy joints? Maybe put down that glass of milk. A study from the University of Central Florida suggests that a bacterium easily acquired by consuming dairy products, beef, or produce grown in cow manure may trigger the development of rheumatoid arthritis (RA) in those who are genetically predisposed to the disease. About 1.3 million adults in the US and 400,000 in the UK suffer from pain, progressive joint deformity, and organ damage associated with RA.
The Cause Of Autoimmune Diseases

The research was based on past findings indicating that irregularities in two related genes called PTPN2/22 increase the risk of the autoimmune disorders Crohn’s disease, Type 1 Diabetes (T1D), and RA. These chronic conditions arise when the body’s defensive cells mistakenly attack its own tissue due to unknown genetic and environmental cues. “If mutations occur in these genes, the PTPN2/22 protein will not function correctly, thus leading to an overactive immune system that leads to autoimmune disorders,” lead author Robert C. Sharp told IFLScience.
Uncovering a Link

Recently, team leader Dr Saleh Naser uncovered a link between the bacteria in question, Mycobacterium avium paratuberculosis (MAP), and both Crohn’s disease and T1D. It appears that the presence of MAP can act like an “on switch” for the abnormal PTPN2/22 in these patients, sending their cell recognition and inflammatory signaling systems into overdrive and cueing the emergence of symptoms. Knowing that RA is also affected by the PTPN2/22 genes, Naser and his co-authors hypothesized that MAP plays a role in this mysterious disease as well.
The First Study
“To our knowledge, this is the first study designed to elucidate the molecular cause of inflammation in RA in association with environmental triggers such as MAP,” the authors wrote in Frontiers in Cellular and Infection Microbiology. They began by analyzing the DNA from blood samples of 70 RA patients and 48 healthy volunteers. Traces of MAP DNA were detected in 34.3 percent of subjects with any type of RA, whereas only 8.3 percent of people without rheumatoid arthritis showed evidence of past exposure to the bacteria.
A Small Mutation Revealed

Sequencing each subject’s risk genes revealed that a small mutation in PTPN2 was present in 78.6 percent of people with RA and 60 percent of people without. Additionally, a mutation specific to PTPN22 was detected in 28.6 percent of RA samples compared with 6.45 percent of healthy controls. “We believe that individuals born with this genetic mutation and who are later exposed to MAP through consuming contaminated milk or meat from infected cattle are at a higher risk of developing rheumatoid arthritis,” Naser said in a statement.
Exposing T-cells to MAP Protein

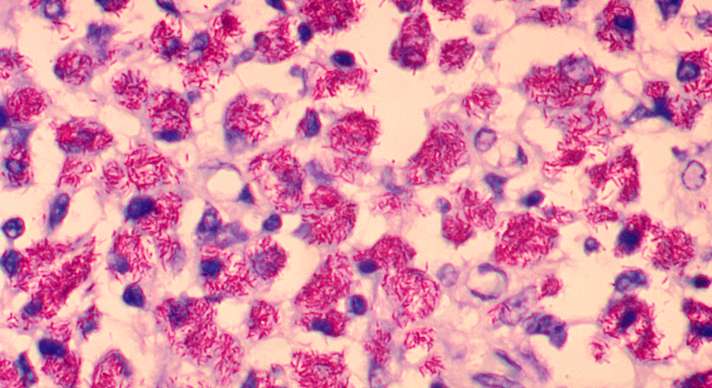
Another telling finding came about by exposing T-cells (a type of lymphocyte that act like the body’s bouncers to identify and remove threats) within the blood samples to a purified MAP protein. Cells from subjects with multiple mutations responded with a frenzy of activity compared to the T-cells from subjects who had RA but did not carry abnormal PTPN2/22 genes. Moreover, the genetically abnormal subjects’ immune cells stayed in overdrive even when the MAP protein was no longer present. In a healthy immune system, cells are supposed to relax from high alert when the perceived threat is neutralized, but those with autoimmune diseases are unable to do so.
The Bottom Line

“We don’t know the cause of rheumatoid arthritis, so we’re excited that we have found this association,” said co-author and rheumatologist Dr Shazia Bég. “But there is still a long way to go. We need to find out why MAP is more predominant in these patients – whether it’s present because they have RA, or whether it caused RA in these patients. If we find that out, then we can target treatment toward the MAP bacteria.”

