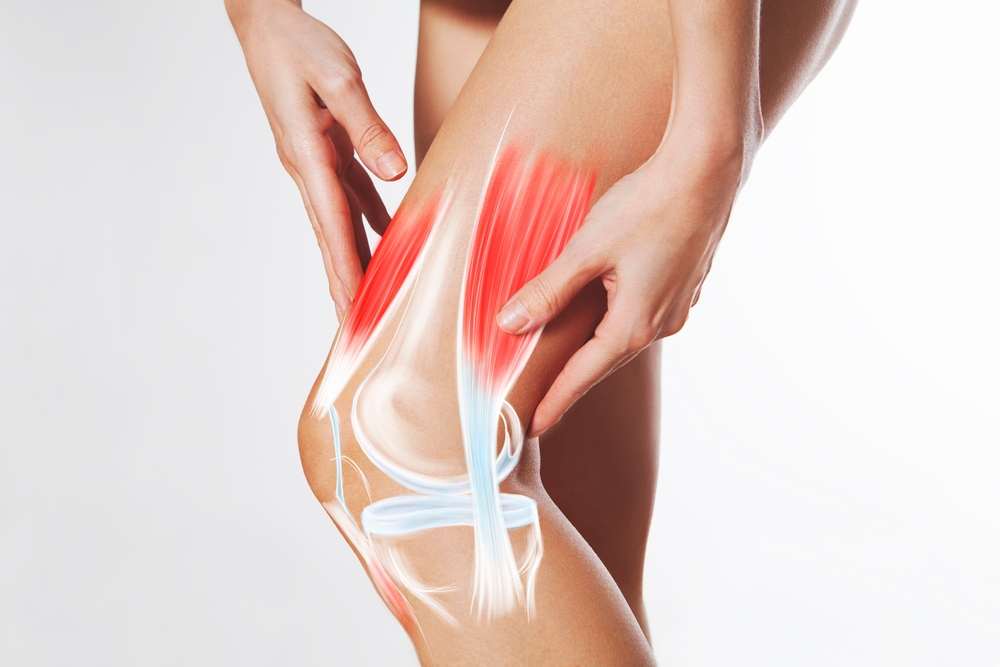
The knee is the largest joint on the body and most prone to issues like injury. A puffy, stiff, or painful knee can limit mobility severely and is extremely painful. While exercise strengthens the knees, if you have a swollen knee it is advisable to consider the root issue. Chronic conditions and acute injuries warrant medical intervention and may be overlooked. Understanding the main causes of a swollen knee helps you treat the problem early and avoid lasting damage. Below, you’ll find seven common culprits followed by clear signs that demand medical attention.
1. Traumatic Injury

A sudden twist, fall, or tackle triggers an inflammatory response leading to a swollen knee. Immediately after the injury, blood flow to the affected area increases to begin the healing process. This process, however, causes the injured area to become inflamed and swollen.
Torn ligaments, especially the ACL, and shredded meniscus cartilage rank among the two most common knee injuries. They stretch or tear tissue, spark an inflammatory response and cause swelling in the injured area.
Recreational athletes face extra risk because rapid direction changes and hard landings put strain on the joint. Early RICE care (rest, ice, compression, elevation) limits swelling, but persistent pain, locking, or instability warrant prompt imaging and perhaps arthroscopic repair.
2. Degenerative or Inflammatory Arthritis

Arthritis affects millions of people globally and is a leading cause of chronic knee swelling. Knees are most affected by two types of arthritis: osteoarthritis or rheumatoid arthritis. Osteoarthritis, the most common form, develops when protective cartilage gradually wears away from joint surfaces.
Rheumatoid arthritis, which is less common, lets immune cells attack the synovial lining.This autoimmune condition causes persistent inflammation that leads to joint damage if left untreated. The swelling often affects multiple joints simultaneously. Aging, obesity, previous injuries, and family history all raise the odds.
Over-the-counter NSAIDs, weight control, structured exercise, and periodic corticosteroid or hyaluronic acid injections reduce flare-ups. When joint space disappears or walking becomes unbearable, orthopedic surgeons may recommend partial or total knee replacement.
Read More: 13 exercises for Knee Pain and Which Ones to Avoid
3. Gout Attacks

Also a form of arthritis, gout occurs when spikes in blood uric acid allow sharp monosodium urate crystals to settle inside joints. This propels swelling and intense redness around the joint area. Although gout usually affects the big toe, it can affect the knee and other joints in the body. Gout occurs especially in middle-aged men, people with metabolic syndrome, and those who down purine-rich diets.
Colchicine, NSAIDs, or short steroid bursts tame acute pain. Long-term control hinges on urate-lowering drugs like allopurinol and lifestyle tweaks that limit beer, organ meats, and high-fructose beverages.
Read More: How To Help Naturally Reverse Gout And Relieve Joint Pain
4. Pseudogout (CPPD Disease)

Calcium pyrophosphate dihydrate deposition disease mimics gout but usually strikes adults over 60. Also known as “false gout”, it differs from gout as it primarily affects the knees and wrists of elderly individuals. Knees and wrists feel the brunt because cooler tissue temperatures favor crystal growth.
Also considered a form of arthritis, pseudogout occurs when a form of calcium crystals build up in joint cartilage and fluid. This build up brings sudden swelling, warmth, and restricted motion. Low-dose NSAIDs or intra-articular steroids ease symptoms, while treating underlying thyroid, kidney, or parathyroid disorders may reduce recurrences.
5. Bursitis
Bursitis develops when small fluid-filled sacs that protect joints called bursae become inflamed and swollen. Also known as “housemaid’s knee,” these sacs normally cushion your knee joint and reduce friction between moving parts. When irritated, they produce excess fluid that creates visible swelling, particularly at the front of your knee. The condition creates a characteristic “bubble” appearance under the skin that may be painful to touch
People who frequently kneel for work, such as carpenters, plumbers, and gardeners, commonly develop knee bursitis. Protective knee pads, activity modification, and short NSAID courses help most cases. Treatment typically involves rest, ice, compression, and anti-inflammatory medications.
Read More: Smoothie To Support Stronger Knee Tendons, Ligaments, and Achy Joints
6. Baker’s Cyst

Baker’s cysts form when excess fluid develops lumps behind the knee. Patients notice a soft lump that tightens during activity and eases at rest. While usually painless, large cysts can limit flexion or even rupture, sending fluid down the calf. These fluid-filled lumps usually cause minimal pain or discomfort.
Underlying knee problems, such as arthritis or meniscus tears, often trigger Baker’s cyst formation. The increased pressure from these conditions forces synovial fluid into the cyst cavity. Many Baker’s cysts disappear on their own once the underlying problem resolves.
7. Lyme Disease

A mysterious bacterial infection, Lyme disease is transmitted through tick bites and can cause knee swelling weeks or months after initial infection. This bacterial infection particularly affects knee joints and can create persistent arthritis-like symptoms. Early antibiotic treatment prevents most long-term complications from Lyme disease though some patients need repeat therapy for lingering inflammation.
When to Call a Doctor

Seek professional care if you cannot bear weight, cannot fully bend or straighten, notice redness spreading or develop chills. Also consult your healthcare profession immediately if the swelling lasts more than 3 days despite applying ice packs or treatment. Early evaluation protects cartilage, uncovers hidden infections, and aids in a speedy recovery.
Seek immediate medical attention if your knee becomes severely swollen, red, and warm to the touch. These symptoms suggest possible infection that requires urgent treatment with antibiotics. Fever, chills, and inability to bear weight also indicate serious problems that need emergency care.
Disclaimer: This information is not intended to be a substitute for professional medical advice, diagnosis or treatment and is for information only. Always seek the advice of your physician or another qualified health provider with any questions about your medical condition and/or current medication. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here.
Read More: 10 Exercises to Help Strengthen Your Knees

