The body is remarkably good at healing. However, some parts of it are more adept than others. One example is cartilage in the knee. It has no direct blood supply, making it harder to mend, and some tears can’t recover without surgery. Now, surgery can stimulate repair or replace cartilage in the knee from another source, leading to a long and often difficult recovery afterward. However, researchers from Northwestern University are developing another solution. They have successfully created a new bioactive material that can regenerate high-quality cartilage in the knees of an animal model.
The Medical Possibilities of Regenerating Cartilage

“Cartilage is a critical component in our joints,” said study author Samuel I. Stupp to Northwestern Now. “When cartilage becomes damaged or breaks down over time, it can have a great impact on people’s overall health and mobility. The problem is that, in adult humans, cartilage does not have an inherent ability to heal. Our new therapy can induce repair in a tissue that does not naturally regenerate. We think our treatment could help address a serious, unmet clinical need.”
In the 2024 study, the researchers administered the material to damaged cartilage in the knee joints of their animal subjects. Within six months, they saw signs of cartilage beginning to regenerate with the natural biopolymers (collagen II and proteoglycans). With further development, the researchers hope the biomaterial could eventually be used to repair injuries like ACL tears, mitigate the need for knee replacement surgeries, and treat degenerative diseases like osteoarthritis.
Read More: Innovative Treatment Heals Spinal Cord Injuries by Triggering Special Proteins
What is in the Biomaterial?
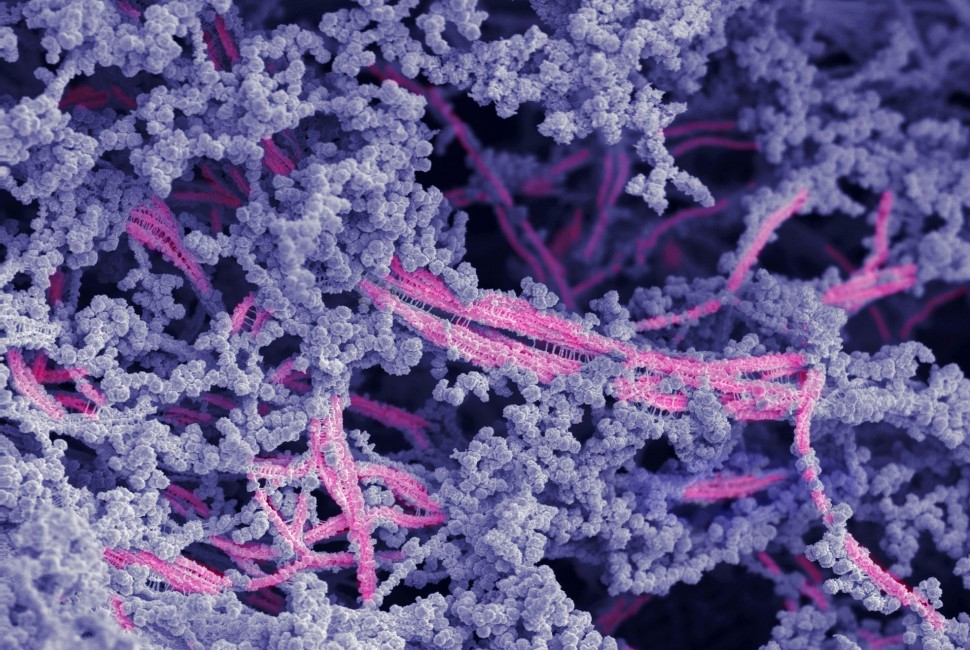
This study is a follow-up to the recent publication from the Stupp laboratory where the authors used molecular motion (which they called “dancing molecules”) to boost the production of proteins that build up damaged human cartilage cells. But in the new study, the team used a hybrid biomaterial instead of dancing molecules. It’s made of two components: a bioactive peptide that binds to a protein vital for cartilage growth, and modified hyaluronic acid, which energizes, supports, and lubricates within in the body.
“Many people are familiar with hyaluronic acid because it’s a popular ingredient in skincare products,” Stupp said. “It’s also naturally found in many tissues throughout the human body, including the joints and brain. We chose it because it resembles the natural polymers found in cartilage.” In the trial, the bioactive peptide and hyaluronic acid particles worked into bundles that mimicked the natural structure of cartilage. The overall goal was to create a platform and signal for the body’s existing cells to regenerate cartilage tissue.
The Test to Regenerate Cartilage
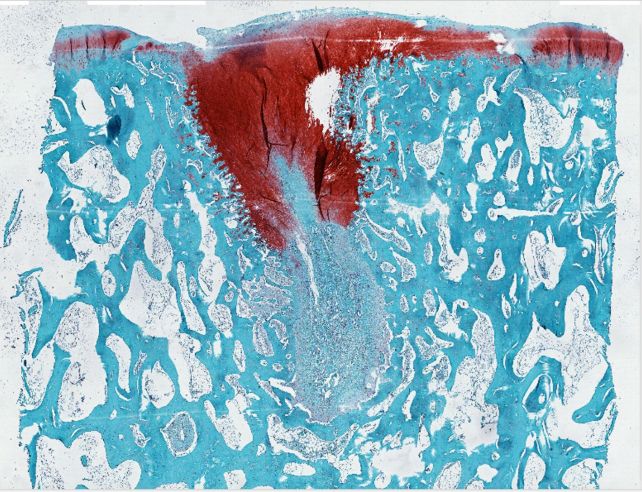
To test the biomaterial’s effectiveness, the researchers use sheep with cartilage defects as the subject. The stifle joints in sheep’s hind legs are similar to a human knee in terms of structure and how they bear weight. Additionally, the cartilage in sheep is especially difficult to regenerate. “A study on a sheep model is more predictive of how the treatment will work in humans,” Stupp said. “In other smaller animals, cartilage regeneration occurs much more readily.” So the researchers injected the biomaterial into the sheep’s defect, and it formed a rubber-like matrix. As the platform disintegrated, new cartilage filled in the gaps. Not only that, the repaired tissue was tested to be of higher quality compared to the control.
The Future of Knee Treatment

Moving forward, Stupp hopes the biomaterial would be able to be applied to joints during open surgeries. This has the potential to be much more effective than current procedures, where surgeons make microscopic fractures on the bone to encourage new cartilage growth, explains MedlinePlus. Another form of treatment is knee replacement surgery, where artificial implants are placed in the leg to alleviate severe pain and mobility issues, says the Mayo Clinic. However, both methods come with challenges, limitations, and potential complications.
“The main issue with the microfracture approach is that it often results in the formation of fibrocartilage — the same cartilage in our ears — as opposed to hyaline cartilage, which is the one we need to have functional joints,” Stupp said. “By regenerating hyaline cartilage, our approach should be more resistant to wear and tear, fixing the problem of poor mobility and joint pain for the long term while also avoiding the need for joint reconstruction with large pieces of hardware.”
Read More: There’s Now an Artificial Cartilage Gel Strong Enough to Work in Knees

