I don’t know about you, but for a long time, I didn’t know what my cervix was or where it was. This was before I found out how dangerous tampons are and started using the menstrual cup. The menstrual cup essentially forced me to find my cervix and become pretty familiar with it. Then, I began using the Fertility Awareness Method (FAM) for birth control, which made me become even more familiar with my cervix on a daily basis.
The cervix is elusive and many women don’t give it much thought. It marks the entrance to our womb and is a few inches in the vagina and feels firm, like the tip of your nose [1]. So without further ado, let’s talk about these 10 facts about your cervix you probably didn’t know!
It’s a Corridor Between Your Vagina and Uterus
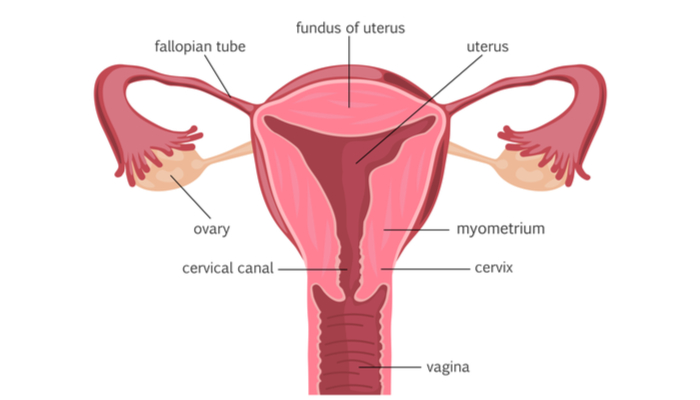
Your cervix connects your vagina and your womb. It produces cervical fluid (sometimes called cervical mucus), which changes as your cycle progresses. For instance, cervical fluid tends to be thick and sticky (infertile) after ovulation, but typically thin and slippery (fertile) before and during ovulation to increase your body’s chances of getting pregnant. This is why the FAM can be difficult to nail down—if you have unprotected sex even days before ovulation if your fluid is fertile, the sperm can survive and basically just be waiting for that egg to appear!
Read More: These Painkilling Cannabis Tampons May Be The End of Period Cramps
It Looks Like a Pink Button That’s Winking at You

It’s likely you’ve never seen your cervix unless you have a speculum, a mirror, and a flashlight. Although I bought a speculum, I still haven’t seen mine because it’s too freaking high most of the time. Fun fact: your cervix moves! (See Fact #9). Your cervix is only about one inch across (3-5 centimeters) and it’s pink, smooth, and fairly firm depending on where you’re at in your cycle.
It Protects Your Uterus and Acts as a Baby Gateway

Many people don’t realize that their cervix actually helps protect the uterus. It decides what’s allowed in (sperm) and what is not (bacteria). During fertile days, it remains open to allow sperm access to the womb, but if you’re not in the fertile part of your cycle, it’s not open for business.
Your cervix has two main functions:
- If you’re not pregnant, it helps keep bacteria from getting further inside the womb.
- If you’re pregnant, it helps to keep the baby in the uterus.
Whether or not you’re trying to get pregnant, your cervix will create a nice, habitable environment for sperm during your fertile days (for most women, this is between 12-19 days after your period begins). This fluid allows sperm to pass through the cervix with the intention of reaching the egg.
It Might Just Make You Climax

Knowing where your cervix is may even improve your sex life, as there’s actually evidence of what are called “c-spot” climaxes from gentle stimulation of the cervix [2]. Stimulation of the cervix will feel better for some women than for others, and it all might depend on how aroused you are, as we’ll soon see!
It Can Get Bruised During Sex

Your cervix can actually get bruised if repeated thrusting occurs during sex. Cervical bruising from sex is often not talked about, but it sounds very painful and uncomfortable [3]. Basically, when you’re aroused, the cervix will retreat to lengthen the vagina and make more room for the penis. This is why having sex when you’re not feeling it can be painful—your cervix may be lower and in the way!
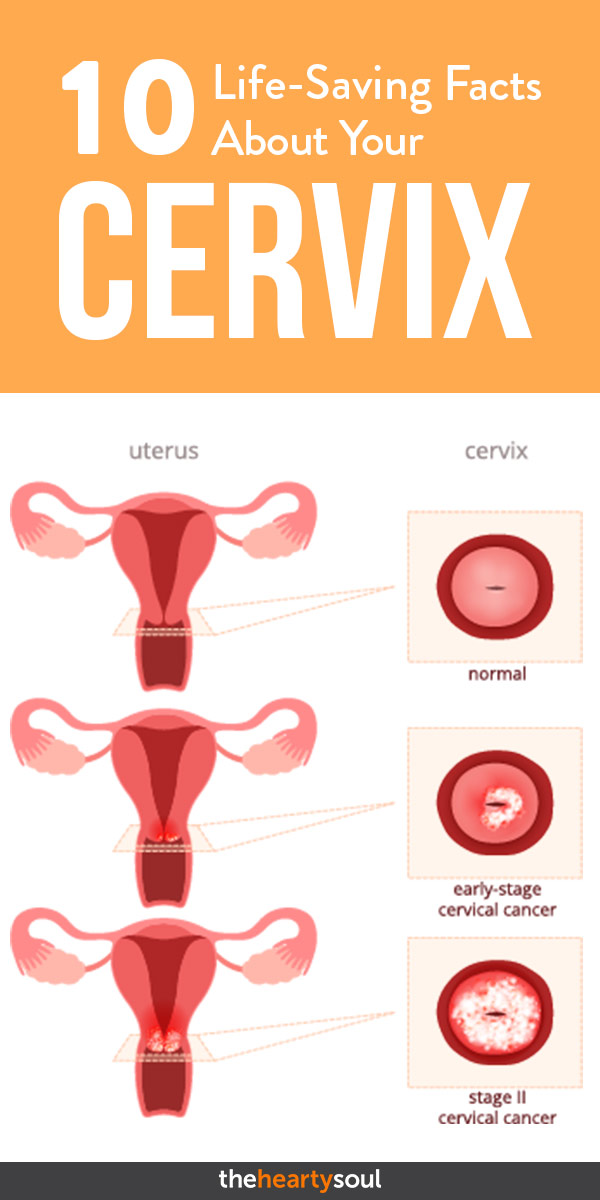
It Can Act as a Marker for STIs and Cancer

Checking the cervix is an important part of pelvic examinations, as the cervix is sensitive to hormones and is often the first area to show signs and symptoms of a disease such as an STI or cancer. Symptoms of either may include an unpleasant odor, strangely-colored cervical fluid, pain during sex, lower abdominal pain, or bleeding in between periods [4]. A PAP smear is used to examine cervical cells for any abnormalities including screening for cervical cancer and human papillomavirus (HPV). A PAP smear is usually conducted every 3-5 years depending on your age [5].
It Can Fall Victim to Disease

Cervicitis is an inflammation of the cervix that may result from an STI, but it may also happen as a result of bacterial overgrowth or an allergic reaction to contraceptives such as the latex in condoms, spermicides, or feminine hygiene products (can we stop using tampons now)?
Since your cervix helps protect the uterus, if it becomes inflamed or infected, there’s a risk that the infection can travel to your womb. Your best defense against cervicitis is to use protection during intercourse to prevent STIs. Symptoms of cervicitis include lots of weird vaginal discharge, painful urination or frequent urination, pain during sex, and bleeding during periods [6].
Read More: Woman Burned From Vaginal Steaming. Is it Worth the Hype?
It Can Act as a Marker of Fertility

We talked about cervical fluid and how it can basically tell you if you’re fertile or not. This fluid is sensitive to estrogen and progesterone. Early in your cycle (called your follicular phase, which starts with your period and ends with ovulation), your fluid will typically be creamy and white.
In the middle of your cycle (ovulation), it will be thinner and clearer, be very stretchy (think egg-white!) and be super cozy with any sperm. If you’re trying to get pregnant, this is your time to have sex! If you’re not trying to get pregnant, your vagina needs to be on lockdown during this time.
Later in your cycle (from the first day after ovulation to the first day of your period, called your luteal phase), your fluid will likely be dry, sticky, crumbly, or maybe still creamy, but it still won’t be a good place for sperm. If you’re interested in using the FAM to prevent pregnancy or just to become more familiar with your cycles, here’s how it actually works.
It’s Susceptible to Cancer

Cervical cancer is the 7th most common cancer in the world [7]. It has the potential for a poor survival rate if it isn’t caught early and spreads to other parts of the body [8]. If caught early, it has a high survival rate, so early detection is important. Although regular screenings are recommended beginning at age 21, there are other things you can do to help curb your risk of cervical cancer. They include:
- Stop taking pharmaceutical birth control. If you’ve been on the pill for 5 years or less, you increase your risk of getting cervical cancer by 10%. If you’ve been on the pill for 5-9 years, you increase your risk by 60%. Your body will take 10 years to return to normal after you stop taking these pills [9].
- Stop smoking. If you’re a smoker, you just doubled your risk of getting cervical cancer.
- Don’t have too many kids. Three or more pregnancies in which the baby is carried to term is associated with a higher risk for cervical cancer, though the reason is unknown.
- Eat more fruits and veggies. This will reduce your risk for many chronic diseases!
Firmness and Position Change
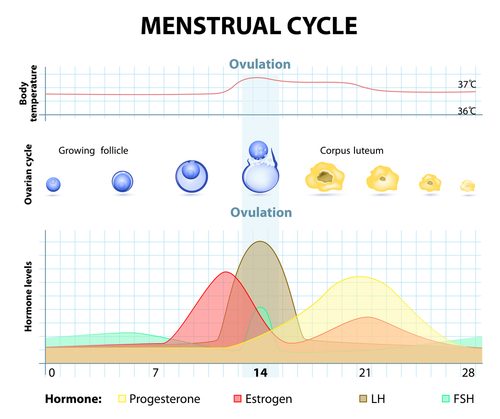
Your cervix can actually move and change its position throughout your cycle, typically staying lower during your infertile days and higher during ovulation. The firmness of your cervix can also change depending on your fertility—during ovulation when your fluid is fertile, your cervix will be much softer and feel open (to let sperm in!), but during your infertile days, it’ll feel firmer and closed.
This makes trying to position your menstrual cup underneath your cervix annoying, as your cervix likes to play hide-and-seek sometimes. If you can’t feel your cervix, it’s best to try and find it in a squatting position, and always wash your hands thoroughly before doing any kind of self-exam down there.
Surprised?

So what do you think? Were you surprised by any of these facts? The cervix is an essential part of our body as women, one that deserves our attention and respect. How familiar are you with your cervix? You may never have a need to “inspect” this part of your body, but acknowledging its role in your health and fertility can help you take the best care of your body!
This amazing post was written by Jenn Ryan, a freelance writer, and editor who’s passionate about natural health, fitness, gluten-free, and animals. You can read more of her work at thegreenwritingdesk.com.
Read More: Sorry Ladies, But It’s Not Supposed to Smell Like Flowers
Sources
- “The cervix.” Canadian Cancer Society
- “Female Sexual Arousal: Genital Anatomy and Orgasm in Intercourse.” NCBI. Kim Wallen, Ph.D. and Elisabeth A. Lloyd, Ph.D. January 17, 2014.
- “Sexually transmitted disease (STD) symptoms.” Mayo Clinic. Mayo Clinic Staff.
- “European Guidelines for Quality Assurance in Cervical Cancer Screening. Second Edition—Summary Document.” NCBI. M. Arbyn,, et al. March 2010.
- “Cervicitis.” Mayo Clinic
- “Worldwide cancer data.” WCRF
- “Cervical Cancer: Statistics.” Cancer
- “Cervical cancer and use of hormonal contraceptives: a systematic review.” The Lancet. Jennifer S Smith, PhD, et al. April 5, 2003.