If you’re a woman reading this, you’re probably aware of the signs and symptoms of breast cancer; however, most women have far less knowledge about cervical cancer, the second most common cancer in women worldwide.(9) Currently, the number of new cases of cervical cases each year is around 500, 000 and it kills 260,000 women annually (11). Despite the prevalence of this type of cancer being high, theoretically, it is completely preventable. Thankfully, knowledge regarding its causes continues to grow rapidly and early intervention and prevention can help in the development of this type of cancer.
What is cervical cancer?

The development of cervical cancer has been linked to a virus called human papillomavirus (HPV), which is transmitted through intercourse. Four out of five women are infected with HPV at some point in their lives without even knowing they have been infected (4). Often, this virus clears by itself due to our immune defenses, however, in some cases, the infection remains and can lead to further health issues. There are many types of HPV and more than 30 infect the genital tract (4). Multiple studies and in-depth research have confirmed the association between certain high-risk strains of HPV and the development of cervical cancer (4).
Read More: What Causes Cancer? 17 Ways to Reduce Your Risk
Signs and Symptoms

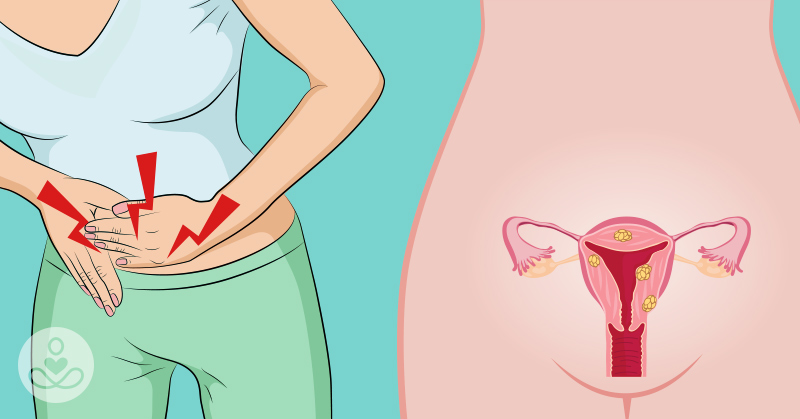
In the early stages of cervical cancer, it is very difficult to know you have it since there aren’t visible symptoms or feelings of discomfort.
With more advanced cases, some clear signs of this disease include:

- Abnormal vaginal bleeding, especially after intercourse.
- Abnormal vaginal discharge
- Pain and discomfort during sex
- Unpleasant odor of genitals
Prevention and Protecting Yourself

Because it is more silent in its development, there is an even greater importance upon being tested regularly. Research into the statistics of this cancer estimates that, this year, in the United States 12,820 women were diagnosed with cervical cancer and 4,210 deaths from the disease will occur (1). These stats are all the more reason to act preventatively against disease development. Two of the most common tests completed to detect cervical cancer early include the PAP test and being tested for the HPV virus (1).
Read More: In World First, Teenage Boy is Cured of Lethal Brain Cancer
1. The PAP test
Or the smear test, looks for pre-cancer cells that may turn into cancerous cells if not treated properly (4). This test is completed at your doctor’s office. Your physician collects a few cells and mucus from the cervix and the surrounding area (4). These cells are then sent to the laboratory to be observed for irregularities. During a PAP test, your doctor may also examine your pelvis or check your uterus and ovaries for abnormalities. A special note to be made is that you should not have your PAP test done while you are on your period.
2. The HPV test

This looks for the virus that can cause changes to those cells (4). This test is usually completed at the same time you are completing your PAP test at your doctor’s office but can be completed alone as well. The same cells collected from your PAP, are tested in a laboratory to see if they are positive for the HPV virus. It is recommended that females begin getting PAP tests and HPV tests at the age of 21 and every 3 years beyond then until the age of 65 (4). That being said, if you have a history of abnormal test results, talk to your doctor about screening more frequently to reduce the risk of disease development.
Because studies have confirmed that cervical cancer is linked to HPV, a significant way women can protect themselves is through safe sex practices, including the use of condoms, to reduce the risk of transmission. For women, charting your cycle to improve body awareness, and making note of any unusual symptoms can also help with early detection of sexually transmitted infections, including HPV.
Treatment

Currently, cervical cancer is treated in several ways depending on what kind and how far along the disease is. It may be treated with surgery, chemotherapy, and/or radiation (1). Your prognosis can greatly depend on your health history, the characteristics of the cancer, and how it responds to certain treatments (1). The 5-year survival rate, which tells you the percentage of women who survive 5 years after being diagnosed, is 68% (2).
Relapse

Recurrent or relapsed cervical cancer occurs in an estimated 35% of those cases of invasive cervical cancer (3). This means it comes back after it has already been treated, either in the same location or in another area of the body (3). The majority of cancer recurrences present within two years of the initial treatment (3).
The Bottom Line

Given that the prognosis of this cancer is quite good if detected early and the fact that it is quite silent in the way it presents itself, it all comes back to early detection and safe sex practices. Take your health in your own hands and check in with your primary healthcare physician or your local female health center to get further informed and to be regularly tested.
Read More: 37-Year-Old Mom Shares Uncommon Early-Warning Sign for Breast Cancer
Sources
- Canadian Cancer Society. (2017). Treatment of Recurrent Cervical Cancer. <https://www.cancer.ca/en/cancer-information/cancer-type/cervical/prognosis-and-survival/survival-statistics/?region=on> Accessed Nov 20, 2017.
- Cancer.Net. (2017).< https://www.cancer.net/cancer-types/cervical-cancer/statistics> Accessed Nov 20, 2017.
- Cancer Treatment Centers of America (2017). Cervical cancer stages. < https://www.cancercenter.com/cervical-cancer/stages/tab/recurrent/> Accessed Nov 20, 2017.
- Centers for Disease Control and Prevention. (2017). What Should I Know About Screening? Retrieved from < https://www.cdc.gov/cancer/cervical/basic_info/screening.htm> Jul 21, 2017.
- Eddy, D.M. (1990). Screening for Cervical Cancer. Ann Intern Med. 113(3): 214-226. <https://annals.org/aim/article/704025/screening-cervical-cancer> Jul 21, 2017.
- Mukama, T. et al. (2017). Women’s knowledge and attitudes towards cervical cancer prevention: a cross sectional study in Eastern Uganda. BMC Women’s Health. 17:9. Retrieved from https://bmcwomenshealth.biomedcentral.com/track/pdf/10.1186/s12905-017-0365-3?site=bmcwomenshealth.biomedcentral.com > Jul 21, 2017
- Munoz, N. & Bosch, F.X. (1989). Epidemiology of Cervical Cancer. IARC Scientific Publications. 94: 9-39. Retrieved from < https://www.popline.org/node/371945>. Accessed Jul 21, 2017.
- Nour, N. M. (2009). Cervical Cancer: A Preventable Death. Reviews in Obstetric & Gynecology. 2(4): 240-244. Retrieved from < https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2812875/>. Accessed Jul 21, 2017.
- Walboomers, J.M.M. et al. (1999). Human Papilloma Virus Is A Necessary Cause of Invasive Cervical Cancer Worldwide. Journal of Pathology. 189: 12-19. Retrieved from < https://www.researchgate.net/profile/Nubia_Munoz/publication/12847339_Walboomers_JM_Jacobs_MV_Manos_M_Bosch_F_Kummer_A_Shah_K_Snijders_PJ_Peto_J_Meijer_CJ_Munoz_NHuman_papillomavirus_is_a_necessary_cause_of_invasive_cervical_cancer_worldwide_J_Pathol_189_12-19/links/554488fd0cf23ff716854167.pdf>. Accessed Jul 21, 2017.
- World Health Organization. Human papillomavirus vaccines. Weekly Epidemiological Record. Geneva; World Health Organization; April 10, 2009. https://www.who.int/wer/2009/ wer8415.pdf. Accessed July 21, 2017.
- World Health Organization. Human papillomavirus vaccines. Weekly Epidemiological Record. Geneva;
- World Health Organization; April 10, 2009. https://www.who.int/wer/2009/wer8415.pdf. Accessed July 21, 2017.